Everything You Need To Know About Meningococcal Disease
June 5 2018About the disease
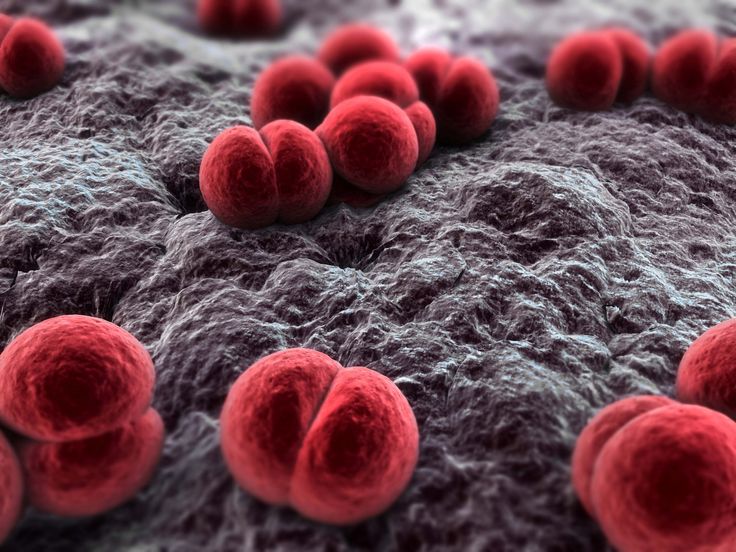
Meningococcal disease is an acute bacterial infection that can cause death within hours if not recognised and treated in time.
In Australia there are 5 main strains of the disease, all of which now have vaccinations available from your doctor.
*Note that the C-strain vaccine available through Australia’s free National Immunisation Program (for children 12 months of age) does NOT protect against all strains of the disease.
Although the majority of victims will recover fully, 10% of those infected will die, and around 20% will have permanent disabilities — ranging from learning difficulties, sight and hearing problems, to liver and kidney failure, loss of fingers, toes and limbs and scarring caused by skin grafts.
Meningitis & septicaemia
One of the reasons meningococcal disease is hard to identify is that it can appear in several different forms, depending on which part of the body the bacteria invade: meningitis (affecting the brain and spinal cord) or septicaemia (affecting the blood), or a combination of both.
Meningococcal meningitis
Meningitis is inflammation of the lining of the brain and spinal cord.
There are many different forms of meningitis — fungal, viral and bacterial. Bacterial meningitis, also called meningococcal disease, is the most serious form.
Symptoms may include a severe headache, fever, fatigue, stiff or painful neck, sensitivity to light or convulsions.
Meningococcal meningitis can result in permanent disabilities – such as deafness or brain injury – and can in some cases cause death.
Meningococcal septicaemia (blood poisoning)
This is the most dangerous and deadly type of meningococcal disease.
It happens when the bacteria enter the bloodstream and multiply uncontrollably, damaging the walls of the blood vessels and causing bleeding into the skin (which results in the distinctive rash).
Symptoms may include fever, fatigue, vomiting, cold hands and feet, cold shivers, severe aches or pain in the muscles, joints, chest or abdomen, rapid breathing, diarrhoea – and, in the later stages, a pinprick or purple bruise-like rash (see Distinctive Rash below).
Septicaemia can lead to death within hours, or permanent disabilities such as severe scarring due to skin grafts and amputation of the fingers, toes, arms or legs – due to lack of blood circulation in the extremities of the body.
Who’s at risk
Meningococcal disease can strike babies, children and adults – anywhere, at any time. Those most at risk are:
- Babies and children up to the age of 5 years – this group accounts for two thirds of cases (due to their less mature immune system and tendency to put things in their mouth and share food, drink and toys).
- Teenagers and young adults from 15 to 24 years – primarily because of the socially interactive lifestyle they lead, which is more likely to involve intimate activities such as kissing.
Winter and early spring are higher risk times, because the many viruses around can weaken the body’s natural immune system. There is also the risk of catching a virus first, followed a few days later by a meningococcal infection, making the illness much harder to identify.
How is it spread?
Meningococcal disease is caused by bacteria (not by a virus), and transmitted via mucus. Meningococcal bacteria can live harmlessly in our throat and nose. Around 20% percent of people will be carrying these bacteria at any one time without ever becoming ill (‘healthy carriers’). In fact, all of us will carry them at some stage in our lives. There are many different strains of meningococcus – since the C-vaccine was introduced, the most common in Australia is now B.
Meningococcal bacteria are not easily spread from person to person and the bacteria do not survive well outside the human body.
The bacteria are passed between people in the secretions from the back of the nose and throat. This generally requires close and prolonged contact with a person carrying the bacteria who is usually completely well. An example of ‘close and prolonged contact’ is living in the same household or intimate (deep) kissing.
Meningococcal bacteria are not easily spread by sharing drinks, food or cigarettes.
Signs & symptoms
Meningococcal disease is a medical emergency. It can kill within hours, so early diagnosis and treatment is vital. Do not wait for the purple rash to appear as that is a critical stage of the disease. Be aware there are two different sets of symptoms, depending on whether it takes the form of meningitis or septicaemia (blood poisoning). A high fever is usually one of the symptoms.
| Common symptoms | Meningitis only | Septicaemia only |
|---|---|---|
|
|
|
Symptoms in babies and young children may include irritability, difficulty walking or lethargy, refusal to eat, a high pitched cry, and a bulging fonteanelle (soft spot on the top of the head).
Distinctive rash
The distinctive meningococcal rash (indicating bleeding into the skin) can be a critical symptom of deadly septicaemia, along with a high fever. The rash may start with a simple spot or blister anywhere on the body, then may progress quickly to red pinpricks like small mosquito bites, and/or spread quickly into purple bruise like blotches. It’s important not to wait until a rash appears before seeking treatment, as the meningococcal rash signifies a critical stage of the disease.
- Get urgent medical advice from your doctor or hospital if you are in any way concerned that you or someone you know is presenting symptoms consistent with meningococcal disease
- If still in doubt or the disease progresses return to the doctor or hospital or seek an urgent second opinion.
- Patients with meningococcal disease need urgent treatment with intravenous antibiotics.
- If the rash appears, in conjunction with other symptoms such as a high fever, call an ambulance for urgent treatment.
- In cases where meningococcal disease is suspected, it is recommended that antibiotic treatment be started before the diagnosis is confirmed by tests.
Vaccination
In Australia there are now vaccines available for each of the 5 main strains of the disease:
Meningococcal C conjugate vaccine protects against meningococcal group C disease. It is recommended for all children at the age of 12 months (as part of the free National Immunisation Program). It is also suitable for teenagers and adults. Contact your GP for more information.
Meningococcal B has 2 vaccines launched in Australia March 2014, and a second in April 2018. Both of which is available by private script from your doctor. Both vaccines are not yet subsidised by the Government. For infants, the vaccine is given in four doses – at 2, 4, 6 and 12 months of age. For children over 12 months, teenagers and adults, the vaccine is given in two doses approximately 2 months apart (for the precise timing, check with your GP). Possible side effects are a mild to moderate fever (as well as a sore arm), so your doctor may recommend giving paracetamol at the same time to babies and children under 5. The new vaccine (launch 2018) has and age indication of 10+ years and two doses required 6 months apart.
Quadrivalent meningococcal conjugate vaccines (4vMenCV) is a combination vaccine and protects against groups A, C, Y and W strains for Meningococcal disease. This vaccine will be included on the NIP (free National Immunisation Program) in the middle part of the year (2018) for babies at 12 months of age.
If you suspect that you or a loved one may have a case of Meningococcal disease, see a doctor or go to the emergency room immediately.
For more information about Meningococcal Disease, visit Meningcoccal Australia.
—
For medical consultations, call to schedule an appointment with us at 03 5229 5192 (Myers Street Family Medical Practice), 03 5241 6129 (The Cottage Medical Centre), 03 5264 8838 (Torquay Medical Health & Wellness Clinic). For Corporate Care Program, visit Workplace Health & Safety Victoria.